Echocardiographic Assessment Of Pulmonary Hypertension
Right ventricular systolic pressure (RVSP) is one important marker, used in combination with other echocardiographic signs, in the assessment of patients at risk for pulmonary hypertension. A tricuspid regurgitant jet of greater than 2.7 m/sec is generally used as the screening velocity for pulmonary hypertension. A Bernoulli equation that incorporates a right atrial pressure estimates the RVSP (RVSP = 4V2 + RAP). Northwest Cardio-Diagnostics (NWCD) has made a committed effort to estimating RVSP when possible, which is demonstrated by the increased likelihood of RVSP being measured in our general patient population (70%) in contrast to a comparable clinic’s general patient population (<50%)[1].
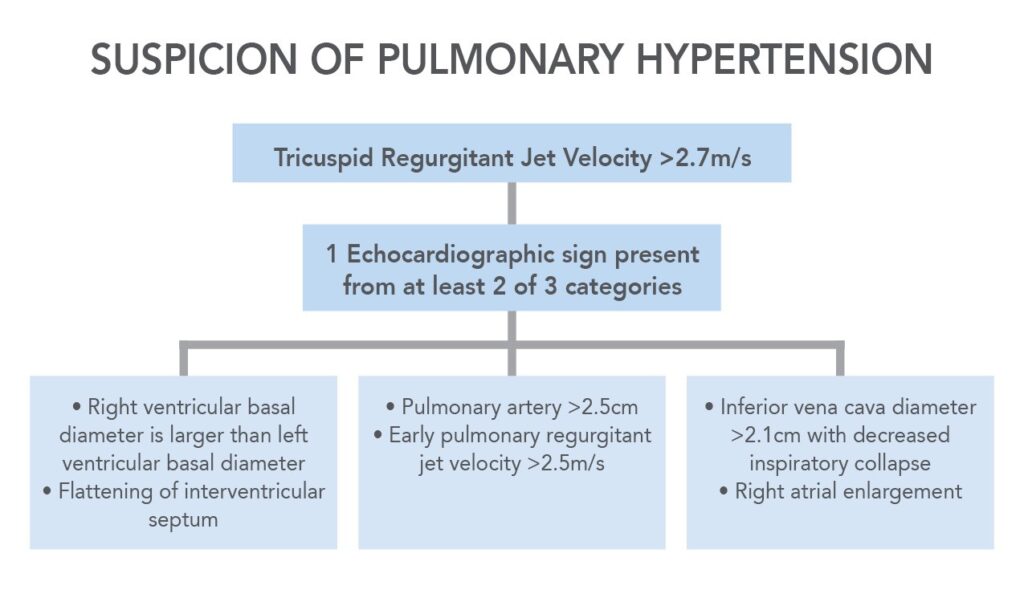
As an elevated RVSP alone does not provide a firm diagnosis for pulmonary hypertension a standard report from NWCD includes other echocardiographic indications of elevated pulmonary pressure, which increase the probability of an accurate diagnosis. When one echocardiographic sign from at least two out of the following three categories are present the probability of pulmonary hypertension is high [2].
A. Right ventricular basal diameter is larger than left ventricular basal diameter.
OR
Flattening of the interventricular septum.
B. Pulmonary Artery Enlargement, > 2.5 cm
OR
Early Pulmonary Regurgitant Jet Velocity > 2.2 m/sec.
C. Inferior vena cava diameter >2.1 cm with decreased inspiratory collapse
OR
Right Atrial Enlargement.
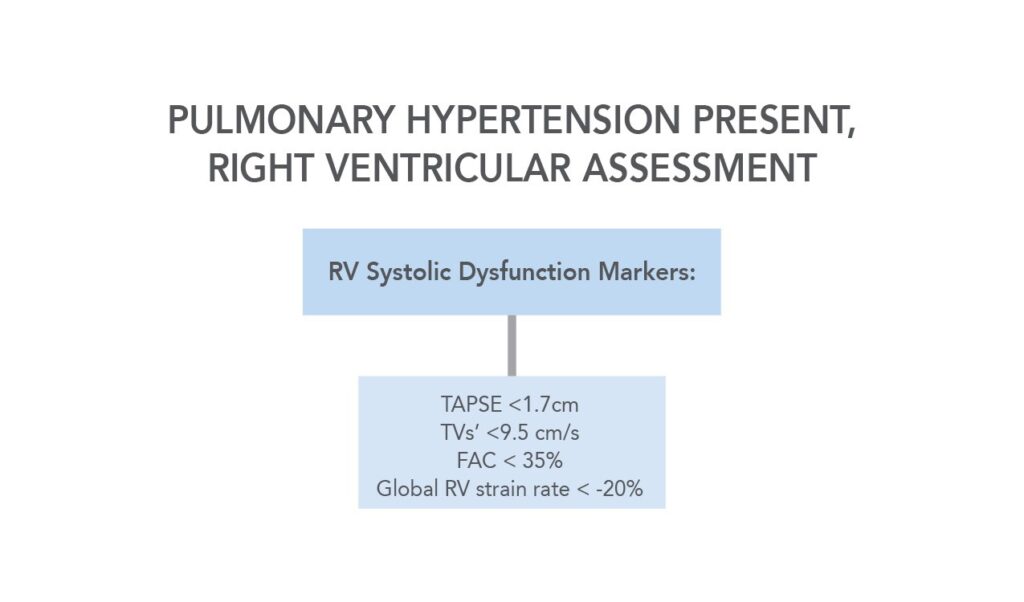
Assessment of the right ventricular (RV) function is a high priority when assessing the severity of pulmonary hypertension. As part of NWCD’s standard reports we include tricuspid annular plane systolic excursion (TAPSE) and peak systolic RV pulsed tissue Doppler velocity taken at the lateral tricuspid annulus (TV S’). TAPSE < 1.7 cm and a TV S’ < 9.5 cm/s indicate RV systolic dysfunction. RV longitudinal strain imaging and Fractional Area Shortening (FAC) are other sensitive indicators of RV function that are included when indicated. A global RV strain rate of < -20% or FAC < 35% quantitatively estimate RV dysfunction. When a pleural effusion is present this is also clearly remarked on.
RVSP has limitations as it requires a detectable tricuspid regurgitant jet, IVC dimension, and may not be reliable in the instance of torrential tricuspid regurgitation or pulmonary stenosis. NWCD does a thorough investigation, using multiple echocardiographic markers to assess the probability of pulmonary hypertension, and is eager to tailor our exams to your specifications.
*NWCD is excellent at accommodating patients who are oxygen dependent or need an elevator. We are a primary clinic used for pre-lung transplant screening and can do an ECG and echocardiogram at the same appointment.
